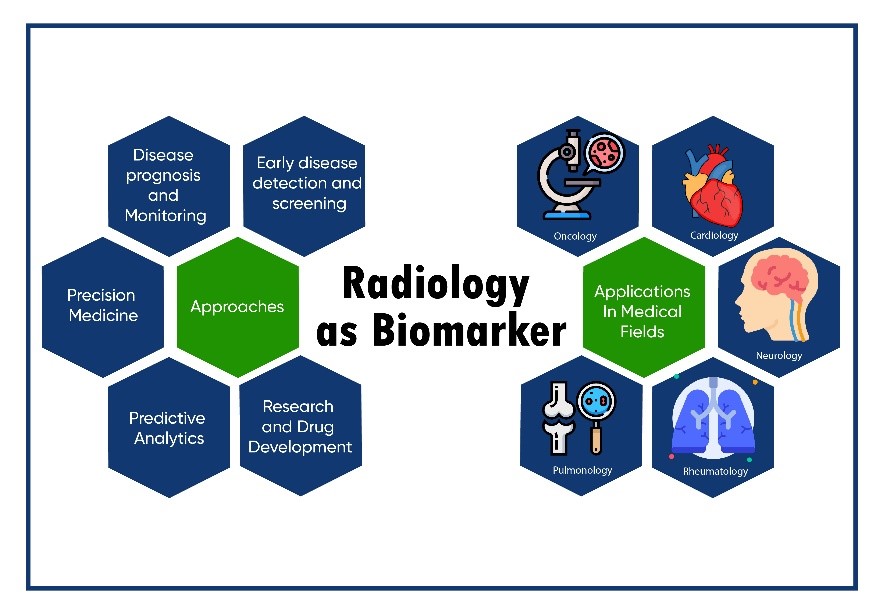
Radiology biomarkers, also called as imaging biomarkers would be mainstay biomarkers in the future. These can detect diseases at an earlier stage, enabling for earlier intervention and therapy. Furthermore, these also provide valuable insight of disease progression and prognostication and treatment response, delivering useful inputs to clinicians. Additionally, radiomics data can create personalized treatment plans, optimizing medication tailored to specific patients. Moreover, AI-powered prediction models can foretell disease outcomes, allowing doctors to make proactive patient care selections.
Radiological biomarkers can be employed in clinical trials to evaluate the efficacy of novel medications and therapies, hence speeding up drug development. A number of imaging biomarker alliances, including the European Imaging Biomarkers Alliance (EIBALL) and the Radiological Society of North America (RSNA) Quantitative Imaging Biomarkers Alliance (QIBA®), are establishing standards for biomarker development, validation, and implementation. Imaging biomarkers are growing increasingly crucial in different medical fields such as cardiovascular disorders, cancer, neurologic and psychiatric disease, musculoskeletal disease, metabolic disorders, and inflammatory and autoimmunity-based disorders. In clinical practice, a variety of imaging biomarkers are being used. For example, Quantitative imaging biomarkers that describe tissue properties include calcium, fat, and iron accumulation, cellularity, perfusion, hypoxia, diffusion, necrosis, metabolism, lung airspace density, and fibrosis and assist in determining the diseased state. CT (or MRI) measures of tumor volume changes in cancer treatment are centered on the “Response Evaluation Criteria in Solid Tumors” (RECIST) criteria.
Nevertheless, the prospect of radiology as a biomarker is enormous, there are several challenges that need to be addressed. Data security and privacy and the requisite for meticulous validation of AI algorithms, ethical considerations with the use of AI in radiology are critical issues. Furthermore, standardization of protocols and guidelines are paramount to assure constancy in radiomics research and clinical applications. Ethical principles and technological improvements must be harmonized for the responsible integration of radiology as a biomarker.
The future of radiology as a biomarker is an invigorating edge in medicine. The world of radiology biomarkers and their integration with radiomics and AI, would bring a paradigm shift in medical diagnosis, improvement in patient care and more personalized treatment and progress in medical research.

