
In the terrain of medical research, clinical trials epitomize as the cornerstone for critiquing the safety and efficacy of novel treatments and interventions. With technological advancement, the huge confines of amassed data become available to the researchers. The imaging data is a pivotal and an invaluable source of information for clinical trials by providing in-depth understanding of the physiological functions of the human body. Albeit, the integration of imaging data into clinical trials upraises innumerable ethical considerations that require vigilant monitoring. This blog provides insights into the ethics that should be taken into consideration while utilizing imaging data in clinical trials. Patient awareness about safety and compensation rights
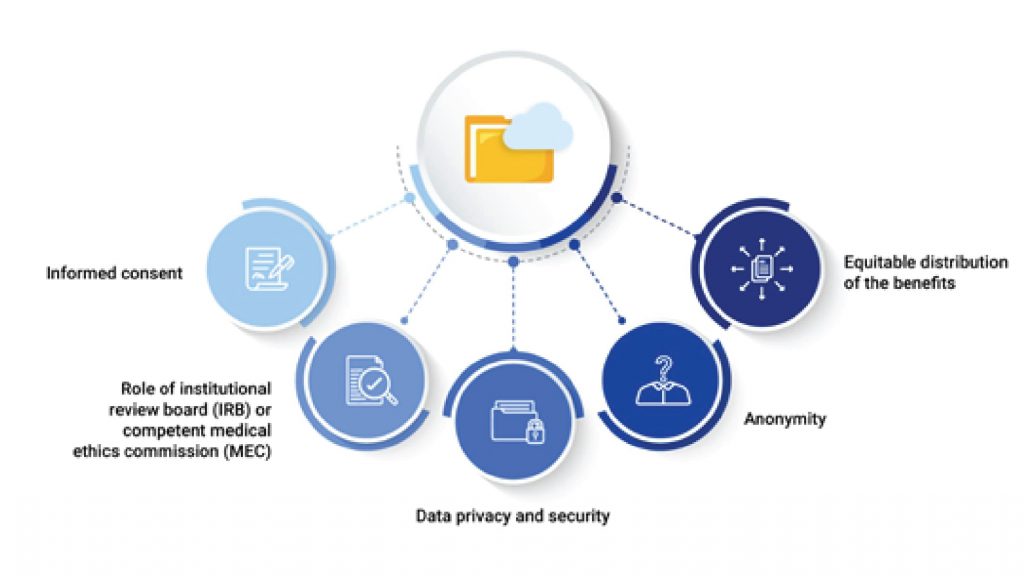
Informed consent
At the forefront of the ethical issues is the principle of patient autonomy. Patients who take part in clinical trials provide researchers access to sensitive imaging data that may reveal particular physical characteristics. The Declaration of Helsinki postulates that: The Declaration of Helsinki was developed by the World Medical Association (WMA) as a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data. After assuring that the potential subject has understood the information, it is imperative that researchers seek the potential subject’s freely-given informed consent, preferably about how imaging data will be used, who will have access to it, and the potential risks, burden and benefits involved, procedures that are implemented in the case of incidental findings. Transparency and clarity are pivotal in fostering trust between researchers and participants.
Role of institutional review board (IRB) or competent medical ethics commission (MEC)
Evaluation of the data collection strategy, continuous monitoring and supervision for the legally and ethically oriented utilization of imaging data in clinical studies are necessary. In India, the necessity of an ethics commission (EC) supervising clinical research was first made in the Indian Council of Medical Research (ICMR) Policy Statement for Ethics published in 1980 and yet later more in the 1988 original Schedule Y edition. Institutional review boards (IRBs) or local competent medical ethics committee (MEC) are authorized to conduct activities in compliance with international ethical guidelines and national laws on medical research and protection of the human rights of subjects and privacy. Since, ethics outlines the fiduciary duties of researchers and medical personnel. It is the responsibility of researchers to follow open and accountable procedures, such as promptly reporting unfavorable events, following study protocols, and abiding by the ethical standards established by regulatory agencies.
Data privacy and security
The usage of imaging data requires robust security and privacy of data from unauthorized access, breaches, and misuse. This includes measures to reduce potential dangers to patient confidentiality and anonymity, such as encryption procedures, restricted access controls, and continuous monitoring. Apart from being ethically and legally essential, the protection of patient privacy is enforced by laws like the Health Insurance Portability and Accountability Act (HIPAA).
Anonymity
All the data used in the clinical trial should be anonymized. All patient names, physicians’ name, hospital and institution names, and other identifying information should be removed from radiology reports to create anonymity. Radiological images can also be rendered anonymous by erasing any embedded text in the image, obscuring patient face in images and deleting additional information, such as serial numbers on surgical implants and devices.
Equitable distribution of the benefits
In order to guarantee that the advantages of imaging data are distributed fairly throughout populations, researchers need to address concerns of diversity and inclusion by involving participants from all the groups of the society. For the sake of greater participation in clinical trials, focused recruiting campaigns, informed consent procedures, and the formation of alliances with community stakeholders should be entailed.
In summary, there is great potential for improving patient outcomes and expanding medical knowledge through the use of imaging data into clinical trials. But this project needs to be led by a strong commitment to moral standards that put patient liberty, privacy, anonymity, equity, and scientific integrity first. By following these guidelines, scientists can use imaging data’s revolutionary potential to spur innovation and raise the standard of care for people all across the world.



0 Comments