
Clinical trials are the foundation of medical advancement. Researchers mostly rely on these trials to determine whether a novel method of therapy or prevention, such as a new drug, diet, or medical device is safe and effective in humans. Clinical research often focuses on finding approaches for early diagnosis of disease, preventing health issues, or enhancing quality of life for those dealing with chronic diseases. An effective clinical data management (CDM) is paramount in order to establish the accuracy, reliability and integrity of research outcomes.
Here in this blog, we examine the value of data management in clinical trials and the essential elements that contribute to its success. The major components of CDM are:
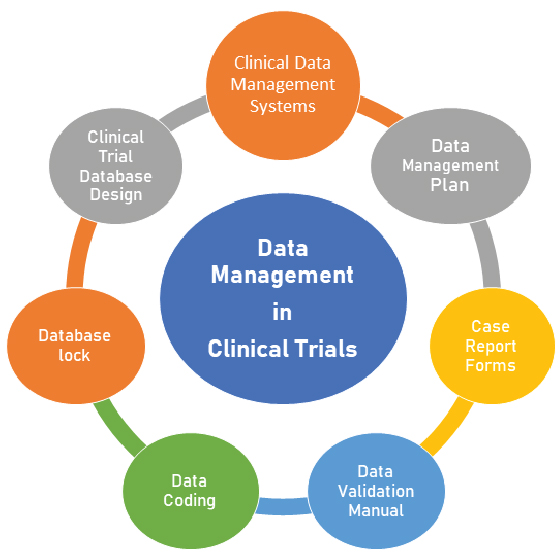
- Clinical Data Management Systems (CDMS) and associated software tools play a prominent role in generating high-quality data by minimizing errors and missing data and gathering as much data as possible for analysis. Some of the open-source tools are OpenClinica, openCDMS, TrialDB, and PhOSCo.
- A well-structured Data Management Plan (DMP) serves as the roadmap for data collection, entry, verification, processing, and analysis throughout a clinical trial. It specifies processes, accountability, and deadlines to guarantee consistency and conformity to legal requirements. The DMP document outlines the CDM guidelines, standards and actions to be carried out during the experiment and provides a roadmap for handling the data in predictable conditions. A more efficient regulatory procedure and compliance are ensured by effective data management. The Good Clinical Data Management Practices (GCDMP) guidelines, which provide the standards of good practice within CDM, were published by the Society for Clinical Data Management (SCDM) in September 2000 initially and revised thereafter several times.
- Case Report Forms (CRFs), an essential component of data management, are standardized printed or electronic forms that are used in clinical trials to gather patient data. A well-designed CRF should be simple to fill out, have a low error rate, robust in content and collect all necessary and study specific data. CRFs should be designed concordantly with the standard guidelines to address the needs of all users such as investigator, site coordinator, study monitor, data entry personnel, medical coder and statistician.
- Data Validation Manual (DVM) another crucial element in CDMS, defines Rules and validation checks for incoming data. This is essential to do early on in the trial to spot and correct data discrepancies or flaws, lowering the likelihood of erroneous results.
- Data Coding is the process of transforming clinical trial data into a standardized format which guarantee consistency in data representation, facilitating comparison and analysis of data across many sites and studies. This is crucial in multi-center investigations in particular. Common coding systems include MedDRA (Medical Dictionary for Regulatory Activities) for adverse events and SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms) for medical concepts. Any medical coding dictionary and all subsequent revisions, having appropriate valid licenses, are loaded in the appropriate coding tool by the database programming team. The coding can be performed in two modes– auto-coding and manual coding.
- A database lock (Study Closeout) indicates the completion of data entry and collecting and stops future data modifications. Before data analysis and reporting, this crucial procedure ensures the stability and integrity of the data.
- Clinical Trial Database Design: To ensure effective data collection and retrieval, the database structure ought to align with the trial’s goals. Data management and analysis are made effortless by a well-designed database.
In addition to ensuring data quality, efficient data management streamlines up the entire clinical trial process, cutting down on expenses and delays. Additionally, it improves patient safety by making it possible to promptly recognize and handle unfavorable situations. CDM even includes the management of various types of clinical and medical images, such as X-rays, MRIs, CT scans, and other diagnostic images. In order to facilitate audit queries and the refiling of applications across regulatory frameworks for various regions or countries, it is imperative to guarantee that clinical and medical data including imaging are efficiently maintained and saved for future data retrieval.
In summary, effective data management is the cornerstone of clinical studies. It guarantees data integrity, compliance with legal requirements, patient safety, effective decision- making, cost management, data security, and long-term research impact. The significance of data management in clinical trials continues to be evident as medical research develops, promising patients throughout the world better and safer therapies.




0 Comments